The Latest Advances in Bladder Cancer Research and Therapy
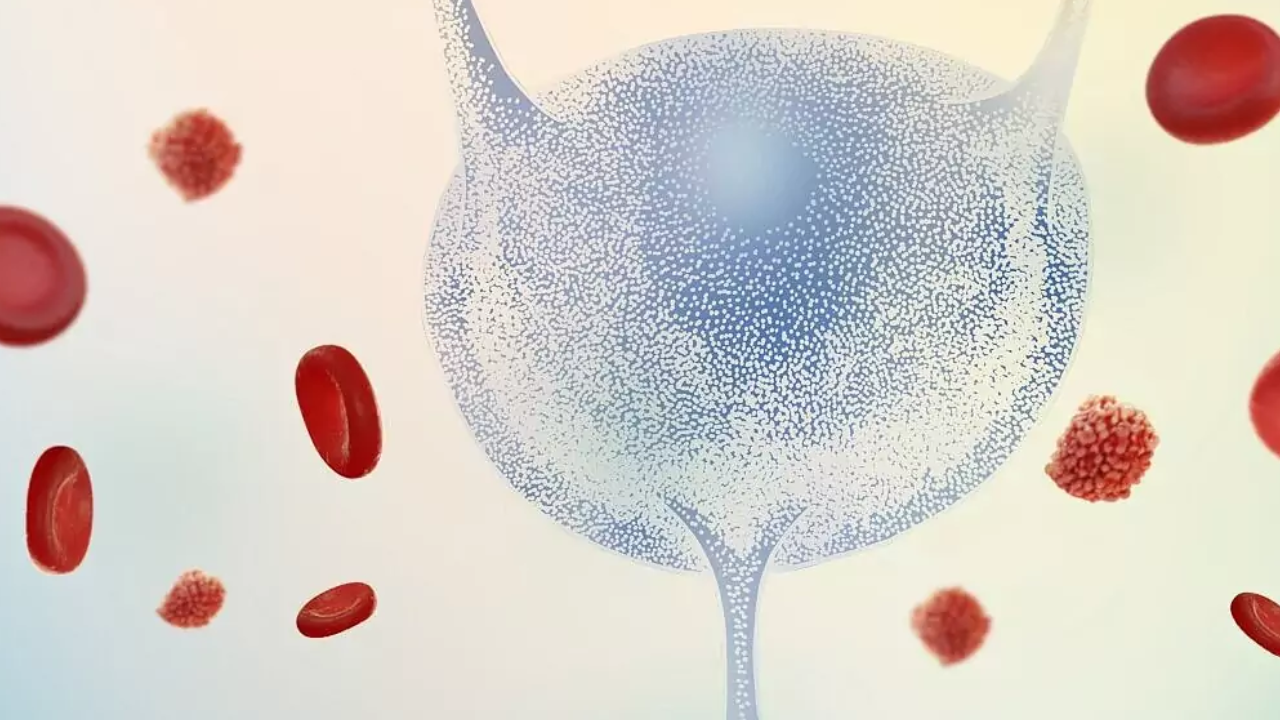
Bladder cancer can have a big impact on someone's life. It's a disease where abnormal cells grow in the bladder, which is a part of the body that holds urine. When someone has bladder cancer, they might experience symptoms like blood in their urine, pain when they pee, or needing to pee often. These symptoms can be uncomfortable and worrying.
But bladder cancer doesn't just affect the body—it can also affect a person's emotions and daily life. Someone with bladder cancer might feel anxious or stressed about their health, and they may need to make changes to their routine, like going to the doctor more often or adjusting their diet. Additionally, treatments for bladder cancer, like surgery or chemotherapy, can cause side effects that impact how someone feels and functions.
However, with the latest advances in research and therapy, there is hope for better treatments and outcomes for people with bladder cancer.
Here are some latest advancements that you may want to discuss with your oncologist:
Minimally Invasive Cystectomy
Minimally Invasive Cystectomy, also known as robotic cystectomy, is a surgery used to remove the bladder in cases of muscle invasive bladder cancer. Unlike traditional open surgery, this procedure involves smaller incisions and the use of robotic technology to assist the surgeon. The robotic instruments are precise and allow for delicate movements, reducing the risk of complications and damage to surrounding tissue.
Patients undergoing robotic cystectomy experience less blood loss, pain, and shorter recovery times compared to traditional surgery. With smaller incisions, patients can often return to their normal activities within three weeks. Overall, robotic cystectomy offers similar success rates with fewer risks and faster recovery.
Expanding Bladder Preservation
Bladder preservation techniques are being explored to help people with muscle-invasive bladder cancer (MIBC) avoid the need for radical cystectomy, a major surgery with significant risks. These techniques, like trimodal therapy (TMT), involve a combination of transurethral resection of the tumor, radiotherapy, and chemotherapy. While TMT is suitable for some patients, it's important to carefully select candidates and monitor their progress closely. Other options, like radical transurethral resection with or without neoadjuvant chemotherapy, are also being studied.
However, there are challenges, including variations in treatment protocols, potential side effects, and long-term outcomes. Collaboration among medical disciplines and patient engagement are crucial for improving bladder cancer care and outcomes.
Immunotherapy Advancements
Immunotherapy, particularly checkpoint inhibitors like pembrolizumab (Keytruda), nivolumab (Opdivo), and avelumab (Bavencio), has revolutionized the treatment landscape for bladder cancer. These drugs have shown efficacy in various settings, including second-line metastatic urothelial carcinoma, locally advanced disease, and adjuvant therapy after cystectomy for high-risk features. Immunotherapy has demonstrated benefits in terms of prolonging overall survival (OS), improving progression-free survival (PFS), and offering better tolerability compared to traditional chemotherapies.
Targeted Therapies
Targeted therapies like erdafitinib (Balversa) have emerged as promising options, particularly for patients with FGFR mutations, which are common in bladder cancer. Drugs targeting specific proteins such as NECTIN-4 have also shown efficacy. For example, enfortumab vedotin (Padcev) is an antibody-drug conjugate that targets NECTIN-4 and has demonstrated effectiveness in clinical trials.
Combination Therapies
Combination approaches, such as the combination of enfortumab vedotin and pembrolizumab, have shown remarkable results in improving survival outcomes for patients with advanced bladder cancer. Clinical trials have demonstrated that these combination therapies can lead to significant increases in overall survival and progression-free survival compared to standard chemotherapy regimens.
Adjuvant Immunotherapy
Adjuvant immunotherapy, such as nivolumab, has shown promising results in preventing disease recurrence after surgery for high-risk bladder cancer. Studies have indicated that post-surgical immunotherapy can significantly prolong disease-free survival, particularly in patients with tumors expressing PD-L1.
Minimally Invasive Surgical Techniques
Minimally invasive surgical techniques, including laparoscopic approaches, are being increasingly utilized in the management of bladder cancer. These techniques offer advantages such as shorter hospital stays and quicker recovery times, potentially making them more accessible to a broader range of patients.
Looking Ahead: The Future of Bladder Cancer Treatment
The future of bladder cancer treatment holds immense promise, with ongoing research focusing on further refining existing therapies and exploring novel treatment approaches.
Additionally, advancements in imaging techniques and biomarker identification are paving the way for personalized treatment strategies tailored to individual patients. Screening protocols are also being developed to enable early detection of bladder cancer, allowing for timely intervention and improved survival rates.
Ongoing research and clinical trials continue to explore novel therapies and treatment combinations aimed at further improving outcomes and quality of life for individuals with bladder cancer.
As we continue to unravel the complexities of bladder cancer and develop more effective treatments, collaboration between researchers, clinicians, and patients remains paramount. Together, we can strive towards better outcomes and a brighter future for all those affected by bladder cancer.
Want to know more an bladder cancer treatments? Book an appointment with KKR hospital oncology specialists and cancer treatment in Chennai.
